Online first
Current issue
Archive
Most cited in 2024
About the Journal
Editorial Office
Editorial Board
Copyright and self-archiving policy
Information clause on the processing of personal data
Declaration of accessibility
Instructions for Authors
Instructions for Reviewers
Contact
Reviewers
2024
2023
2022
2020
2021
2019
2018
2017
2016
2015
2014
2013
Editing and translations
ORIGINAL PAPER
Association between brain fog, cardiac injury, and quality of life at work after hospitalization due to COVID-19
1
Jagiellonian University Medical College, Kraków, Poland (Department of Neurology)
2
University Hospital in Krakow, Kraków, Poland (Department of Neurology)
3
Jagiellonian University Medical College, Kraków, Poland (Department of Periodontology, Preventive Dentistry and Oral Medicine, Institute of Dentistry, Faculty of Medicine)
4
Jagiellonian University Medical College, Kraków, Poland (Department of Pharmacology)
5
John Paul II Hospital, Kraków, Poland (Department of Cardiac and Vascular Diseases)
Online publication date: 2024-02-27
Corresponding author
Marcin Wnuk
Katedra i Klinika Neurologii, Uniwersytet Jagielloński Collegium Medicum, Kraków, Jakubowskiego 2, 30-688, Krakow, Polska
Katedra i Klinika Neurologii, Uniwersytet Jagielloński Collegium Medicum, Kraków, Jakubowskiego 2, 30-688, Krakow, Polska
Med Pr Work Health Saf. 2024;75(1):3-17
KEYWORDS
TOPICS
ABSTRACT
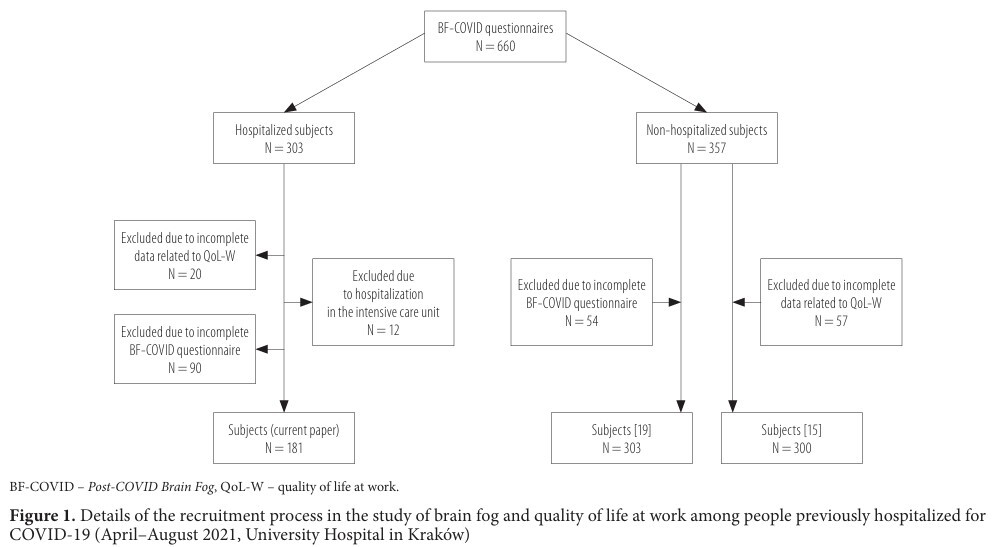
Background: To evaluate incidence and search for possible predictors of brain fog and quality of life at work (QoL-W) among low-to-moderate risk subjects previously hospitalized due to COVID-19. Material and Methods: Participants aged ≥18 retrospectively reported 8 brain fog symptoms pre-COVID-19, at 0–4, 4–12 and >12 weeks post-infection via validated clinical questionnaire. The QoL-W was assessed with a 4-point Likert scale where 0, 1, 2, and 3 meant no, mild, moderate, and severe impairment in performing activities at work, respectively. Data on age, sex, comorbidities, and laboratory results (including first in-hospital high-sensitivity cardiac troponin I [hs-cTnI] measurement) were gathered. Results: The study included 181 hospitalized subjects (age Me = 57 years), 37.02% women. Most had low disease severity (Modified Early Warning Score = 1, 77.90%) and low comorbidity (Charlson Comorbidity Index 0: 28.72%, 1–2: 34.09%), with no intensive care unit treatment needed. COVID-19 led to almost 3-fold increased brain fog symptoms, with incidence of 58.56%, 53.59%, and 49.17% within 4, 4–12, and >12 weeks, respectively (p < 0.001). First in-hospital hs-cTnI levels were 47.3% higher in participants who later presented with brain fog at median follow-up of 26.7 weeks since the diagnosis of the SARS-CoV-2 infection. Individuals who experienced at least one brain fog symptom at follow-up, had elevated hs-cTnI, less often presented with atrial fibrillation, and used anticoagulants during initial hospitalization due to COVID-19. The Hs-cTnI >11.90 ng/l predicted brain fog symptoms in multivariable model. COVID-19 was associated with 3.6‑fold, 3.0‑fold, and 2.4-fold QoL-W deterioration within 4, 4–12, and >12 weeks post-infection (p < 0.05). Subjects with QoL-W decline >12 weeks were younger, mostly women, had more brain fog symptoms, and higher platelet counts. Multivariable models with self-reported brain fog symptoms (responding coherently and recalling recent information), age, and sex exhibited good discriminatory power for QoL-W impairment (area under the receiver operating characteristic curve 0.846, 95% CI: 0.780–0.912). Conclusions: This study highlighted that in non-high-risk subjects hospitalized during the first 2 pandemic’s waves: 1) brain fog was common, affecting nearly half of individuals, and impacting QoL-W >12 weeks after initial infection, 2) after 3 months of COVID-19 onset, the decline in QoL-W was primarily attributed to brain fog symptoms rather than demographic factors, health conditions, admission status, and laboratory findings, 3) components of brain fog, such as answering in an understandable way or recalling new information increased the likelihood of significantly lower QoL-W up to tenfold, 4) biochemical indicators, such as the first hs-cTnI level, might predict the risk of experiencing brain fog symptoms and indirectly decreased QoL-W >12 weeks after COVID-19 onset. Occupational medicine practitioners should pay particular attention to younger and female subjects after COVID-19 complaining of problems with answering questions in understandable way or recalling new information as they have an increased risk of QoL-W impairment. Med Pr Work Health Saf. 2024;75(1):3–17
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.